6.4K
Downloads
27
Episodes
This podcast is about the advancement of rare disease research told by health professionals, researchers, parents, and advocates. This podcast is for you to learn how newborn screening research saves the lives of babies every day through discoveries of new technologies and treatments. You will hear stories from experts who treat babies, the families who care for them, and the researchers who make it all happen.
Episodes

Monday Sep 25, 2023
Innovative Blood and Marrow Transplant & Gene Therapy for Rare Diseases
Monday Sep 25, 2023
Monday Sep 25, 2023
Dr. Paul Orchard is the Medical Director of the Inherited Metabolic and Storage Disease Program and a Professor in the Department of Pediatrics in the Division of Blood and Marrow Transplant & Cellular Therapy (BMT & CT) at the University of Minnesota. He is interested in using hematopoietic stem cell transplantation (HSCT) and other cell therapies, including gene therapy, to improve outcomes. In addition to his clinical work with patients with inherited metabolic diseases, Dr. Orchard is engaged in research designed to identify strategies that enhance the delivery of enzymes to the brain and the peripheral nervous system for patients who lack specific enzymes. Other interests include the modification of stem cell transplant approaches and combination therapies to improve outcomes for patients with inherited diseases and the potential to develop multi-institutional cooperative studies for these disorders. Listen to a leading expert in saving the lives of children every day, including Dr. Amy Brower's son.

Thursday Aug 31, 2023
Lifting the Voices of the Community in the Rare Disease World Through Storytelling
Thursday Aug 31, 2023
Thursday Aug 31, 2023
If you need a boost of inspiration, a bit of laughter, and a lot of intention, listen to our special guest on the Newborn Screening SPOTlight podcast Effie Parks, who transformed her experiences raising a son with a rare disease to helping others by sharing their stories on her podcast, Once Upon a Gene. The best way to describe Effie may be as the rare disease parent’s best friend… and greatest resource!
She was born in Montana, where she was raised with her 12 siblings. After moving to Washington and marrying her husband, they were blessed with the birth of their son, Ford Canon Parks. When she learned that Ford had been born with an extremely rare genetic condition – CTNNB1 syndrome – she immersed herself into the world of advocacy. Now, she is the host of her own podcast, Once Upon a Gene, where she speaks to others about their journey through life with rare disease. Since the launch of the podcast, Once Upon A Gene was awarded “Best In Show Podcast” by WEGO Health. Podcast Magazine recognized Effie as one of the 40 Under 40 Podcasters and she has been nominated for two Champion of Hope awards from Global Genes. Her mission is to learn, lift voices of the community, connect people to resources and to leave this world better than she found it for others in the rare disease world.
Interview Questions:
You are the host of podcast of Once Upon a Gene, where you speak to others about their journey through life with rare disease. Your mission is to learn, lift voices of the community, connect people to resources and to leave this world better than you found it for others in the rare disease world. What inspired you to start your podcast?
- Your baby was diagnosed with a rare disease called CTNNB1 syndrome. Can you tell us what led to the diagnosis and what happened next?
- Researchers discovered the genetic testing for CTNNB1 syndrome. While there is no single treatment for CTNNB1 Syndrome, each of the symptoms associated with the syndrome may be treated. Also, CTNNB1 gene is a good candidate for genetic replacement therapy. This exciting to hear the new development and research in treatments. Could you share your process in caregiving to your child with CTNNB1 syndrome? Any advice for new moms?
- Newborn screening identifies metabolic and genetic disorders at birth. Before your child was diagnosed with CTNNBI, were you aware of newborn screening?
- What do you think prospective parents should know about newborn screening?
- You are the host of Once Upon A Gene podcast, can you tell us what inspired to start the podcast?
- On your Once Upon a Gene blog, you shared that the movie “Back to Future” and especially the main cast member, Michael J. Fox have inspired you. Can you elaborate in what ways to our listeners?
- What has been going on in your life recently that you expected and didn’t expect?
- As you know NBSTRN creates tools and resources to help stakeholders to advance newborn screening research. How could NBSTRN and other organizations such as the Rare Diseases Clinical Research Networks supported by the National Center for Advancing Translational Sciences (NCATS) help you and your community to advance rare disease awareness?
- Where can people go to learn more about you? What can people expect from you next?
- What is one final thought that you want to leave our listeners with?
- What does newborn screening research mean to you?
Monday Jul 31, 2023
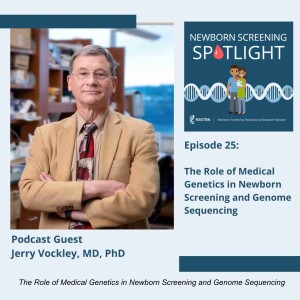
The Role of Medical Genetics in Newborn Screening and Genome Sequencing
Monday Jul 31, 2023
Monday Jul 31, 2023
Join us on the Newborn Screening SPOTlight podcast with Dr. Jerry Vockley, who is a Professor of Human Genetics, the Graduate School of Public Health, Cleveland Family Endowed Pediatric Research, School of Medicine, Chief of Genetic and Genomic Medicine, UPMC Children’s Hospital of Pittsburgh, and Director of the Center for Rare Disease Therapy, UPMC Children’s Hospital of Pittsburgh.
Dr. Vockley is internationally recognized as a leader in the field of inborn errors of metabolism. His current research focuses on mitochondrial energy metabolism, novel therapies for disorders of fatty acid oxidation and amino acid metabolism, and population genetics of the Plain communities in the United States. He has published over 320 peer-reviewed scholarly articles and is the principal or Co-investigator on multiple NIH grants. Dr. has an active clinical research program and participates in and consults on multiple gene therapy trials.
Dr. Vockley has served on numerous national and international scientific boards including the Advisory Committee (to the Secretary of Health and Human Services) on Heritable Disorders in Newborns and Children where he was chair of the technology committee. He is a Fellow in the American Association for the Advancement of Science. He is a Founding Fellow of the American College of Medical Genetics and Genomics, and currently serves on its board of directors. He is founder and chair of the International Network on Fatty Acid Oxidation Research and Therapy (INFORM). He has served as chair of the Pennsylvania State Newborn Screening Advisory Committee and is a past president of the International Organizing Committee for the International Congress on Inborn Errors of Metabolism and the Society for the Inherited Metabolic Disorders (SIMD).
On this podcast, Dr. Vockley shares his career journey and personal stories about the impact of newborn screening research on physicians, families, and advocates.
Interview Questions:
- Among your many appointments, you serve on the Board of the American College of Medical Genetics and Genomics (ACMG) and advise on efforts to improve health through the practice of medical genetics and genomics. In addition to the ACMG board, you were integral in the early and current days of the NBSTRN. Can you tell us how you got involved in NBSTRN?
- As technologies to screen, diagnose, treat, and manage disease advance and increasingly use sequencing, can you share with our listeners your vision of how sequencing will be used in newborn screening in the future? What excites you about this potential, and can you share any concerns?
- You have published over 320 peer-reviewed scholarly articles and led many efforts funded by NIH and others. Can you describe the key findings from your most recent publication, “Rapid Whole-Genomic Sequencing and a Targeted Neonatal Gene Panel in Infants With a Suspected Genetic Disorder.”
- You are the Cleveland Family Endowed Pediatric Research, School of Medicine Professor of Human Genetics, Graduate School of Public Health, and the Director of the Center for Rare Disease Therapy, UPMC Children’s Hospital of Pittsburgh. In your article titled “Scaling genetic resources: New paradigms for diagnosis and treatment of rare genetic disease,” you mentioned that the movement from the basic science laboratory to clinical trials is still hampered by a regulatory system rooted in traditional trial design and requires a fresh assessment of safe ways to obtain approval for new drugs. You proposed the development and scaling of nucleic acid-based therapies. Could you share this possibility with our listeners and what challenges need to be overcome to deliver them safely with appropriate evaluation and long-term follow-up?
- Can you share any stories of inspiration that keep you going?
- Anything else you’d like to share?
- Thank you for your efforts in conceptualizing the NBSTRN and establishing a network of stakeholders that includes health professionals, researchers, state programs and families, and advocates. Do you have advice for this community and how they can help to realize and capitalize on the fifteen years of NBSTRN?
- You are involved in training the new generation of medical geneticists. What do you tell them about newborn screening research?
- What does NBS research mean to you?
Friday Jun 30, 2023
Friday Jun 30, 2023
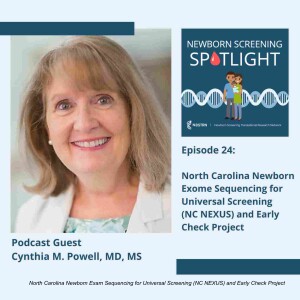
Today, on the Newborn Screening SPOTlight podcast, we are thrilled to have Dr. Cynthia Powell join us to share her vision of genomic sequencing in newborn and her experience as the Past Chair of the U.S. federal Advisory Committee on Heritable Disorders in Newborns and Children. Dr. Powell is a Professor of Pediatrics and Genetics at the University of North Carolina at Chapel Hill School of Medicine, where she sees patients, teaches students, residents and fellows, and participates in research. She is a board-certified clinical geneticist, cytogeneticist, pediatrician and genetic counselor. She completed her pediatric residency at Children’s National Medical Center in Washington, D.C. and medical genetics fellowship at Children’s National Medical Center and the National Institutes of Health.
She is the program director of the UNC Hospitals Medical Genetics and Genomics Residency Program. She is the immediate past Chair of the U.S. federal Advisory Committee on Heritable Disorders in Newborns and Children and a member of the Board of Directors of the American College of Medical Genetics and Genomics.
She is Past President of the Association of Professors of Human and Medical Genetics and the American Board of Medical Genetics and Genomics. She serves on the North Carolina Newborn Screening Advisory Committee and the North Carolina Genetics and Genomics Advisory Committee. Her research interests include newborn screening, genomics, birth defects and genetic syndromes. She led the North Carolina Newborn Exome Sequencing for Universal Screening (NC NEXUS) project, a five year project funded by NIH investigating the utility of next generation sequencing in newborns.
She is the UNC site principal investigator for the Early Check project, a voluntary newborn screening research project in North Carolina that offers parents the opportunity to have their infant screened for conditions that are not yet part of standard public health newborn screening. She currently serves on the NBSTRN Steering Committee and has contributed to the development of tools and resources for newborn screening research. Dr. Powell wears many hats in her different roles in medical genetics and newborn screening. You will be inspired by her story of dedicated commitment in improving the lives of children.

Tuesday Jun 06, 2023
Living with Phenylketonuria (PKU) and Caring for Patients with PKU
Tuesday Jun 06, 2023
Tuesday Jun 06, 2023
This episode features Brittany Holmes who is a nurse practitioner in the Metabolism Program in the Genetics & Genomics division at Boston Children’s Hospital. She is an experienced provider who specializes in caring for patients with inborn errors of metabolism. She serves on the Board of Directors for the National PKU Alliance, the Newborn Screening Translational Research Network (NBSTRN) Steering Committee, and the Rare Disease Clinical Research Network (RDCRN) PHEEFREE Consortium External Advisory Board.
She received her Bachelor of Science at Merrimack College, and Master of Science in Nursing from Simmons University in Boston, and is beginning the Doctor of Nursing Practice program at UMass Boston this September. In addition to expanding expertise in the clinical care and research for those with a variety of inborn errors of metabolism, she also has a particular interest in Phenylketonuria (PKU) and newborn screening. Her interest in working with inborn errors of metabolism began at a young age, due to her personal experience as a patient with PKU. After years of speaking at conferences from the patient perspective and receiving care from leading clinicians/researchers in metabolism from the patient side, this ultimately led to seeking a career as a healthcare professional in the specialty. She enjoys being able to offer both the provider and patient perspective, and has a passion for caring for patients in this specialty.
Interview Questions:
- Could you tell our listeners how you got involved in newborn screening?
- May is the PKU awareness month. What is the purpose of this rare disease awareness campaign. How can our listeners get involved this month?
- In the year 2023, it is the 60th anniversary of the newborn screening, and PKU was the first condition to be screened in newborns in 1951. A PKU screening test is a blood test given to newborns one to three days after birth. If babies are identified with PKU, they can benefit from early treatment. However, in the year 2013, there was a study that indicated that there is individual patient, social, and economic factors prevent some adult PKU patients in the US from accessing treatment. Ten years later, do you see any changes?
- There is a policy in development or in place to address this such as The Medical Nutrition Equity Act (MNEA). Can you tell us listener about this policy?
- In addition to medical nutrition therapy for PKU patients, what are other new types of treatment and gene therapy for PKU patients? Could you share the latest research effort and clinical trial in this area?
- You are on the Rare Disease Clinical Research Network (RDCRN) PHEEFREE Consortium External Advisory Board. What is the mission and activities of this network? What resources are available to patients and families with rare disease?
- Could you share your process for proving medical care to patients with PKU? As an adult with PKU, any advice for new parents who just received a newborn screening positive result for PKU?
- What do you think prospective parents should know about newborn screening research in screening, diagnosis, and treatment for PKU?
- You are currently on the Steering Committee at NBSTRN, what efforts do you see NBSTRN can support in NBS Research and your efforts?
- What does NBS research mean to you?

Saturday Apr 29, 2023
Advocacy Work for Newborn Screening Research and Treatment for Sickle Cell Disease
Saturday Apr 29, 2023
Saturday Apr 29, 2023
Every state screens for sickle cell disease and researchers are working with industry and advocates to develop new ways to improve the health outcomes of individuals living with sickle cell disease.
Today, on the Newborn Screening SPOTlight podcast, we welcome Yvonne Carroll, RN, JD who is trained as a researcher, a lawyer, a nurse, and a patient advocate and is currently the Director of Patient Services in the Department of Hematology at St. Jude Children’s Research Hospital in Memphis, Tennessee. She has over two decades of dedicated commitment to advancing the management of care, advocacy work for equitable resources, and community engagement to amplify the voices of patient and families with sickle cell disease.
She sits on several editorial and national boards including the National Black Nurses Association (NBNA) Sickle Cell Sub-Committee, the International Association of Sickle Cell Nurses and Professional Associates (IASCNAPA), and the Sickle Cell Community Consortium Executive Board.
Yvonne been appointed and reappointed as a member of the Tennessee Governor’s Genetic Advisory Committee for more than 15 years, and has been involved in community based participatory research since the beginning of her career, and in 2021, was recognized by American Lebanese Syrian Associated Charities (ALSAC), which is the largest healthcare related charity in the United States, with the St. Jude Legacy Award for her lifetime work with the sickle cell community.
Yvonne graduated with a Bachelor of Nursing Degree from the University of Tennessee and a Law degree from the University of Cincinnati. She is a proud veteran of the U.S. Navy, Judge Advocate General Corps, and is a wife, mother, and grandmother. Join us in listening to Yvonne share her passion and inspiring story of hope and vision for newborn screening research in sickle cell disease.
Podcast Interview Questions:
- How did you get involve with newborn screening research.
- You are currently the Director of Patient Services in the Department of Hematology at St. Jude Children's Research Hospital in Memphis, Tennessee. Can you tell our listeners about your role? (Yvonne, you can mention about the St Jude SCRIPP program and listeners can learn more about it here).
- You have been funded for sickle cell disease projects for more than 20 years. What areas of research have advanced in sickle cell disease as well as stalled in these past decades? Where do you see the direction of newborn screening research in sickle cell disease in the future?
- Your work also involved in engaging and empowering families in decision making process on the management of care for sickle cell disease. What advice do you have for researchers to engage families and advocacy organization to amplify their voices?
- You were a part of a group who published a study on “Strategies to increase access to basic sickle cell disease care in low- and middle-income countries”. Can you tell share with our listeners on these helpful strategies needed to increase access to basic SCD care for patients in these settings?
- You presented on “Informed Consent for Sickle Cell Disease Gene Therapy Reimagined” at the NBS Research Summit hosted by NBSTRN last September 2022. What are current challenges in consent process? How do you envision the informed consent reimagined?
- Are you involved in training the next generation of advocates and nurses, and what do you tell them about newborn screening research? (Yvonne, you can talk about Sickle Cell Nursing Bootcamp and include links and application process).
- You are currently on the Steering Committee at NBSTRN. What role do you see NBSTRN play in helping to advance your work and the field of sickle cell diseases?
- What does NBS research mean to you?

Friday Mar 10, 2023
Friday Mar 10, 2023
We are thrilled to have Dr. Stephen Kingsmore, a dedicated physician, researcher, an inventor, and who is the currently the President/CEO of Rady Children's Institute for Genomic Medicine in San Diego, California. In this podcast, you will not only learn what drives Dr. Kingsmore’s purpose to improve the lives of newborns and to prevent avoidable and unnecessary deaths due to late diagnosis of rare genetic condition, but also his challenges in clinical practice and research in making his dream of a learning healthcare system using genomic medicine a reality globally. Among his achievements, Dr. Kingsmore pioneered the development of ultra-rapid Whole Genome Sequencing to decode rare disease in newborns. In 2021, he led the RCIGM team to break his own world speed record by achieving diagnosis via WGS in 13.5 hours. Dr. Kingsmore came to Rady Children’s in 2015 from Children’s Mercy Kansas City, where he was the Executive Director of Medical Panomics. He previously served as President and CEO of the National Center for Genome Resources; COO of Molecular Staging Inc.; Vice President of Research at CuraGen Corporation; founder of GatorGen; and Assistant Professor at the University of Florida’s School of Medicine. Dr. Kingsmore received MB, ChB, BAO and DSc degrees from the Queen’s University of Belfast. He trained in clinical immunology in Northern Ireland and did residency in internal medicine and fellowship at Duke University Medical Center. He is a fellow of the Royal College of Pathologists. Learn from Dr. Kingsmore how to work through the challenges in research and clinical practice in advancing newborn screening research.
Podcast Interview Questions
- Thank you, Dr. Kingsmore, for being a guest on the NBSTRN podcast, NBS SPOTlight. We are excited to speak with you today! Dr. Kingsmore, you are currently the President/CEO of Rady Children's Institute for Genomic Medicine, where you lead a multi-disciplinary team of scientists, physicians and researchers who are pioneering the use of rapid Whole Genome Sequencing to enable precise diagnoses for critically ill newborns. How did your interest in rare disease research lead you to San Diego?
- Many of us remember specific milestones you and your team have accomplished and your calls to action have inspired stakeholders across the NBS community. During your presentation at our NBS Research Summit in 2021 you spoke about “NBS and Rapid Whole Genome Sequencing (rWGS) for Severe Infant Onset Genetic Diseases". Most recently, you were a part of the International Conference on Newborn Sequencing (ICoNS) in augural meeting where you joined researchers from across the world to share information about newborn sequencing initiatives. What were the major takeaways from that meeting, and what should the NBS Research Community be aware of?
- You recently published that your team has developed a “Scalable, high quality, whole genome sequencing from archived, newborn, dried blood spots.” Up to eighty-one genetic diseases are included in screening, thirty-six of which are recommended for NBS by a federal advisory committee known as the Recommended Uniform Screening Panel. As you know, there are more than 7,000 rare genetic diseases (RD) that affect 6-8% of the US population or about 30 million Americans. Addition to the RUSP is a lengthy process. What are your thoughts on how the use of genome sequencing using dried blood spots to identify rare diseases could change the landscape of newborn screening policy when we currently adopt one condition at a time and the nationwide implementation can take years?
- We appreciate your contribution to the American Journal of Medical Genetics Special Issue on Newborn Screening Research, where Dr. Amy Brower and Dr. Kee Chan were co-editors of this issue. Your article on the “Dispatches from Biotech beginning BeginNGS: Rapid newborn genome sequencing to end the diagnostic and therapeutic odyssey” highlights the BeginNGS, a consortium in collaboration with academia, pharmaceuticals, biotechnology and non-profit organization to provide a platform for implementing whole-genome sequencing for newborn screening, disease management and interventions, and rare disease drug development for use by partners around the world. Could you share the work in progress as of now?
- If we were to implement whole-genome sequencing for newborn screening globally one day, how do you envision long-term follow-up of management of care for the patient and families, including medical, non-medical, psychological services, education, and other related services to improve the quality of life to be supported?
- You received your medical training from the Queen’s University of Belfast in Ireland. You trained in clinical immunology in Northern Ireland and did residency in internal medicine and fellowship at Duke University Medical Center. You are also a fellow of the Royal College of Pathologists. What sparked your interest in newborn screening?
- You have such a long history of successes and accomplishments that have global impact on health care and public health. In March of 2015, you surpassed your previous record in genetic sequencing by reducing the process to 26 hours, which was recognized in April 2016 by Guinness World Record as the fastest genetic sequencing in the world. Now, I think your team has reduced the time again. On the flip side of the coin, would you mind sharing your biggest challenge —and what did you learn from that experience?
- What’s your biggest challenge in your research right now, and how are you tackling it? How could NBSTRN data tools and resources assist you?
- What does NBS research mean to you?

Monday Feb 27, 2023
Monday Feb 27, 2023
For the rare disease community, there is a common motto “alone we are rare, together we are strong”. Advocacy organizations play this important role in connecting families of rare disease , amplifying their voices and helping to improve health outcomes for people living with rare diseases. Today’s podcast guest is Annie Kennedy who has over three decades of experience in advocacy work. A veteran leader in the rare disease patient advocacy movement, Annie joined the EveryLife Foundation in 2018, where she led the National Economic Burden of Rare Disease study, the development of the ICD Code Roadmap, and the community-driven Guide to Patient Involvement in Rare Disease Therapy Development. Annie previously held leadership roles at Parent Project Muscular Dystrophy (PPMD) and the Muscular Dystrophy Association (MDA). She is a sought-after advisor to patient-centered organizations and initiatives across the nonprofit and government sectors. If you are new to advocacy work or a seasoned advocate, become inspired by Annie’s story to carry forward despite the road to advocacy work is non-stop, exhausting and at times, bumpy with many ups and down. Join this collective energy to advocate for rare diseases research.
Podcast Interview Questions:
1. For over three decades your advocacy work has been critical to amplifying the voices and you are currently the Director of Chief of Policy, Advocacy, & Patient Engagement for the EveryLife Foundation for Rare Diseases. Can you share with our listeners the mission of the EveryLife Foundation? What were major accomplishment made? And how can they get involved?
2. EveryLife Foundation for Rare Diseases also plays important roles in advancing newborn screening advocacy in the United States. What is your vision for how stakeholders across newborn screening and the rare disease community can work together?
3. EveryLife Foundation led a study to assess the total economic burden of 379 rare diseases in 15.5 million individuals in the United States in 2019. The total economic burden was $997 billion. What were your key takeaways from this important study and how can the results inform researchers, clinicians, policy makers, and other key stakeholders?
4. Prior to the EveryLife Foundation, you were involved in the Parent Project Muscular Dystrophy (PPMD) and the Muscular Dystrophy Association (MDA). In that time, you helped lead the legislative efforts around passage and implementation of the MD-CARE Act (2001, 2008, 2014), the Patient Focused Impact Assessment Act (PFIA) which became the Patient Experience Data provision within the 21st Century Cures Act (sec 3001). Congratulations, these are incredibly impactful efforts. Can you tell our listeners about the ‘behind the scenes’ activities that were undertaken to lead these efforts and the implementation strategy.
5. February is a special month. Every year, last day of February is a day to raise awareness for rare diseases and improve access to treatment and medical representation for individuals with rare diseases and their families. What are some rare disease day activities taking place?
6. Are you involved in training the next generation of advocates, and what do you tell them about newborn screening research?
7. How did you know leading advocacy work was your calling? Can you share your career journey?
8. The road to advocacy work is non-stop, and at times, bumpy, do you have any stories of inspiration that keep you going?
9. How can NBSTRN assist in you advocacy work?
10. What does NBS research mean to you?

Thursday Jan 19, 2023
Thursday Jan 19, 2023
Listen to Dr. Wendy Chung, a board-certified clinical and molecular geneticist with over 20 years of experience in human genetic research, share her story. Her team has led ground-breaking research describing the genetic basis of both rare and common genetic diseases, and the development of precision therapies based on the genetic findings in individuals. She was a part of the two-year pilot of newborn screening for Duchenne Muscular Dystrophy and is currently leading the GUARDIAN STUDY, which has a goal of genome sequencing 100,000 newborns in NYC. She is currently the co-Chair of NBSTRN Steering Committee, which has informed the evolution of the tools and resources for newborn screening research.
Podcast Interview:
- Dr. Chung, you are a board-certified clinical and molecular geneticist with 20 years of experience in human genetic research. How did you get involved with newborn screening research?
- Your work has led to ground-breaking publications describing the genetic basis of both rare and common genetic disease, and your efforts have often described not only the basis for disease, but the development of precision therapies based on the genetic findings in individuals. You are now leading a new effort, the Guardian Study. Please tell our audience how your years of research led you to conceive of and undertake this effort.
- NBSTRN highlights innovative efforts at our annual NBS Research Summit. You presented in 2020 on the "Genomic Causes of the Broken Hearts” Can you describe your goals with this effort and how this could facilitate early treatment and improve health outcomes for infants with congenital heart disease?
- Your research team collaborated with ACMG and NBSTRN, and many others in a two-year pilot of newborn screening for Duchenne Muscular Dystrophy. Could you share with our listeners what you and the consortia learned from this pilot and how this might inform future efforts?
- In 2019 the NBSTRN Bioethics and Legal Workgroup led a published recommendations to guide pilot studies and included a recommendation to enroll diverse participants. Informed by this work, your team examined parental views about expanded NBS and the use of genomics. Please tell what this effort told you about the role of parental choice in expansion of NBS.
- Are you involved in training the next generation of board-certified clinical and molecular geneticist and what do you tell them about newborn screening research?
- Thank you for serving as co-chair of the NBSTRN Steering Committee. What are you most excited about? What role could NBSTRN play in your efforts in advancing NBS research?
- In addition to funding NBSTRN, NICHD supports a variety of efforts to advance NBS research. CDC and HRSA also fund important efforts to advance and support NBS through work with state NBS programs, policy makers, parents and advocates. Please share your vision of how these key federal partners could work together to accelerate the translation of research findings into public health and clinical care.
- What does NBS research mean to you?

Tuesday Dec 20, 2022
Tuesday Dec 20, 2022
Family engagement and rare disease advocacy drive the innovations and accelerate the discoveries that advance newborn screening research. Today, we are excited to have Natasha Bonhomme, a health communications strategy and family engagement expert who has led ground-breaking initiatives to empower individuals, families, and their communities to transform health care. Natasha is currently the Chief Strategy Officer for Genetic Alliance and the founder of Expecting Health, a national effort to create outreach strategies and deliver educational programming to diverse communities, with a special emphasis on maternal and child health issues. A decade ago, Natasha and her team launched Baby’s First Test as the first National Newborn Screening Resource Center to provide education, family support and services information, and resources about newborn screening at the local, state, and national levels. Natasha received her BA in Psychology from Boston College and began her career as a summer intern at NIH. This year, 2022, her journey from intern to national expert was recognized as Natasha and received the Judi Tuerck Newborn Screening Follow-up and Education Award for her significant contributions. Listen along with us as she shares advice on engaging families and educating the next generation of advocates to help speed research to develop new technologies to screen, diagnose, treat, and manage the disease. Newborn screening saves lives, and leaders like Natasha help make it possible!
Interview Questions:
1. Congratulations on receiving the Judi Tuerck Newborn Screening Follow-up and Education Award at the APHL NBS Symposium. This award honors someone who has made significant and outstanding contributions in providing innovative newborn screening follow-up training/education for best practices. This year recipient is you, Natasha. You are the founder of Expecting Health and chief strategy officer, Genetic Alliance. Baby first test is a part of the Expecting Health, and it has been 10 years. For our audience, could you share the mission of Expecting Health and how they can learn more?
2. You have a new program called Parent Navigators. Can you tell us about this program and why it is important?
3. You are also the Chief Strategy Office of Genetic Alliance. Can you share with our audience your role and the mission of Genetic Alliance? How did you get involved with newborn screening research?
4. Your work involved engaging and empowering families in the decision-making process on maternal and child health issues. In the era of expanding newborn screening with additional conditions on the RUSP and the potential of using genomic sequencing, what are family perspectives towards genetics, and what are the challenges that researchers need to reconsider in conducting public health genetics and genomic research?
5. What advice do you have for researchers to engage families and advocacy organizations to amplify their voices and concerns in the design of their research study?
6. Newborn screening tests are conducted by the State Newborn Screening Program. Can you describe an example of large-scale education for newborn screening? Do you have tips on partnering with the state program?
7. UCSF recently published an article titled “Non-White Newborns With Cystic Fibrosis More Likely To Be Missed in Screening.” Your work has intersected the area of diversity, equity, and inclusion. What do you think we as an NBS Research Community need to do?
8. Are you involved in training the next generation of advocates, and what do you tell them about newborn screening research?
9. What does NBS research mean to you?
